About the framework
In response to this global public health emergency, the Scottish Government has commissioned the development of an education framework on AMR and AMS for non-specialist health and social care staff (i.e. those staff who do not have a dedicated role in AMS). Although intended as a framework for health and social care in Scotland, it may have applicability in other UK nations.
Aims of the framework
Staff groups
Domains, subdomains and topics
How can this framework be used?
Implementation
Other related frameworks
Values and behaviours
Aims of the framework
This multidisciplinary framework supports the following strategies and action plans:
- The Infection Prevention Workforce: Strategic Plan 2022 – 2024
- Scottish Healthcare Associated Infection (HCAI) Strategy 2023 – 2025
- UK 5-year action plan for antimicrobial resistance 2024 to 2029.
The framework aims to support staff to play their part in coordinated action, individually and as part of a team. It covers the knowledge, skills and behaviours staff need to contain and control AMR within their job role and play an active part in safeguarding antimicrobials for the future.
Everyone can contribute to this without being an expert or specialist, even if it is just one action.
The framework aims to achieve the following:
- Raise awareness of the issue of AMR amongst Scottish health and social care staff and students.
- Highlight the need for coordinated action.
- Support collaborative practice/teamwork and joint decision-making.
- Help staff and students to contribute to managing and reducing AMR in their roles.
- Support employers/recruiters to assess transferrable skills and identify required behaviours that contribute to safeguarding antimicrobials.
- Support educators in creating appropriate learning resources, training sessions, etc.
It can be used by individual workers and teams, organisations and education providers.
Antimicrobial Stewardship – A care journey
This framework has a broad scope and looks at AMR and AMS through the lens of a care journey. It highlights where in the journey staff can contribute to keeping antimicrobials and those in their care safe. Everyone can play a part, for example by:
- keeping those in care and their families/carers well informed
- monitoring those receiving antimicrobial treatment
- making sure antimicrobials are taken correctly, not forgotten and disposed of safely.
Staff groups
The framework covers very broad groups of staff and students:
- everyone working or preparing to work within health and social care in Scotland, who interacts/will interact with those in care or their families/carers
- those who are involved in direct care or in a supporting role
- laboratory staff who provide diagnostic expertise and laboratory reports which are essential for the treatment of infections
- staff in management and organisational oversight roles who can influence and direct the provision of services.
It excludes any additional competencies for staff in specialist antimicrobial stewardship/infection roles. Examples for these roles are antimicrobial stewardship nurses, antimicrobial pharmacists, infection specialist doctors and nurses and those with non-prescribing specialist infection roles in laboratory medicine and public health/epidemiology.
But this framework will be useful for those new to a specialist post in AMS/IPC. Specialists/leaders will also find the framework useful to identify learning needs in their wider team and for signposting or directing those who are thinking about working in the field or are interested in developing specialist competencies. All AMS/IPC/Health Protection specialists should be familiar with this framework.
The framework covers all care settings, from primary care to hospitals, from care homes to care at home. The content of the framework is generic, and statements have not been aligned to a specific care setting.
The applicable staff groups for each statement in the framework are only indicative. There are many different roles in many different health and social care settings, with varying individual and local responsibilities. But they all can play an important part in keeping those we care for safe. Staff are unlikely to fit neatly into one of the framework columns. They should discuss areas for development with their manager/supervisor.
Staff group definitions
Defined as staff in supporting health or social care roles who interact with those in care or their carers, but who are not involved in direct care. Examples are receptionist, medical secretaries, porters transporting those in care, etc. These are staff who might speak to those in care, or their families or carers, answer questions, receive requests or complaints, etc.
Non-prescribers of antimicrobials
Defined as staff/students who provide direct care to people, e.g. by dispensing and administering antimicrobials, monitoring treatment or caring for people with infection, but do not prescribe antimicrobials.
This includes:
- Staff/students from services related to antimicrobial stewardship (laboratory staff from microbiology or virology laboratories, pharmacy staff)
- All registered nursing and midwifery staff/students
- Other staff/students with many different roles and from different care settings, e.g. allied health professionals, dental nurses, clinical healthcare support workers, care home or home care support workers. However, not all statements will apply to all of these staff/students.
Defined as medical and non-medical prescribers, e.g. medical and dental students, medical doctors, and dentists. This group also includes other health and social care staff who have completed an accredited prescribing course and registered their qualification with their regulatory body, for example pharmacists, nurses, midwives, and allied health professionals.
Health or social care staff in management roles
Defined as staff who do not provide direct care but can influence antimicrobial stewardship in a managerial or organisational oversight role. This includes staff who have health and social care organisational or public health responsibilities and those who manage health and care services and undertake activities that can support antimicrobial stewardship. This includes those with health and social care roles in e.g. procurement, strategic planning and policy development, and non-executive and executive health board members.
Domains, subdomains and topics
Domains provide the main structure of the framework. Some domains have been divided into sub-domains to aid navigation. Each domain/subdomain is divided into different topics.
This framework includes domains/topics that highlight knowledge, skills and behaviours that directly contribute to keeping antimicrobials safe. These include infection prevention and control (IPC), vaccination, the diagnosis of infection, clinical decision making, diagnostic stewardship, communication, education, collaborative practice and management.
Each domain has a main broad competency statement. This is then followed by knowledge, skills and behaviour statements for each topic.
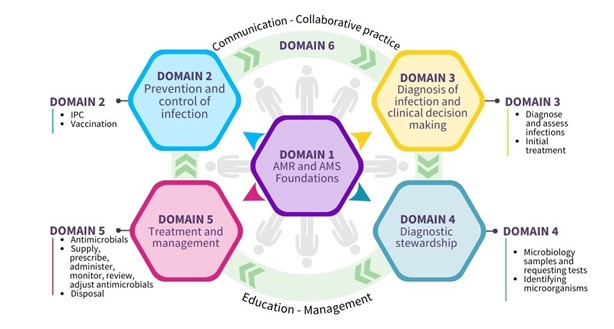
Fig. 1: Domains and subdomains
Domain 1: Foundations - awareness of antimicrobial resistance and antimicrobial stewardship
This domain covers the underpinning knowledge of AMR and AMS. It recognises that staff need to understand the impact of AMR and the importance of AMS. They need to see the links between AMR, AMS and IPC, and their role before they can effectively contribute to keeping antimicrobials safe.
Domain 2: Prevention and control of infection
IPC and vaccination are critical first steps in limiting the use of antimicrobials and the development of AMR. If we prevent avoidable infections, then we limit antimicrobial use and resistance. This includes viral infections that may be confused with (or predispose to) bacterial infection. The domain covers basic IPC knowledge, skills and behaviours staff need to support AMS.
Domain 3: Diagnosis of infection and clinical decision-making
This domain emphasises the importance of recognising and being able to identify if someone has an infection as early as possible. Clinical decision making includes distinguishing between colonisation and infection. It is also important to understand how clinical investigations help with the diagnosis of infections and which initial treatment options to consider.
Domain 4: Diagnostic stewardship
This domain is about using appropriate laboratory or near patient testing. Choosing the right test for the right person at the right time will reduce unnecessary testing and reporting. This supports appropriate treatment, optimises clinical outcomes, and ultimately limits AMR.
Domain 5: Treatment and management - appropriate use of antimicrobials
This domain is a key part of the framework and covers key characteristics of antimicrobials and what to consider when using them. The way we treat and manage those we care for impacts on limiting AMR and reducing adverse events. This includes both empirical treatment (based on knowledge, experience and empirical guidelines, before we have a confirmed diagnosis) and treatment once laboratory results are available. It involves the supply, prescription, administration, monitoring, review, adjustment of therapy, and disposal of antimicrobials according to best practice guidelines. It also highlights the importance of non-antibiotic measures in infection management and recognising when treatment can safely be stopped.
Domain 6: Communication, education, collaborative practice and management
The domain covers effective communication with colleagues, those we care for, their families and carers. It includes managing expectations and educating others about the safe use of antimicrobials. Promoting and prioritising AMS is also part of this domain.
How can this framework be used?
The framework can be used flexibly to direct and support learning and development of students, front line staff and managers. It applies across a very wide range of settings. It can also suit local contexts and circumstances at an individual, team, service and organisational level. It should be used in line with other appropriate frameworks.
The framework is first and foremost a tool for identifying and addressing learning needs. It does not need to be read from cover to cover. Instead, users should look at the domains and topics of the care journey in Figure 1, assess which of them apply to their job role or the intended target audience and where there is a need for learning and development.
The framework aims to provide support and guidance for learning and development on AMR and AMS. It is not prescriptive.
It aims to be a tool to support the following:
Individual staff members/students:
- Identify knowledge, skills and behaviours for their role in health and social care.
- Identify knowledge and skills areas to discuss with a manager/supervisor during a personal review.
Line managers/supervisors/teams:
- Assess if there is a need for individual or team development.
- Highlight in conversations with staff their role and contribution to AMS in practice.
- Discuss the importance of AMR and AMS during appraisals.
- Encourage staff to undertake personal development to improve their knowledge and skills.
Organisations:
- Identify and highlight the required knowledge and skills during recruitment.
- Create specifications for the commissioning of any bespoke education and training.
Education and training providers:
- Analyse the content of existing AMR and AMS education and training resources to identify any gaps.
- Check other education and training resources and identify areas where references to AMR and AMS can be included to increase awareness.
- Create bespoke training resources and interventions to support specific staff groups.
The following questions will help to navigate to an appropriate part of the framework:
- Staff group: Which of the main staff groups indicated is most appropriate for the staff member/target audience as a starting point?
- Domains/subdomains: Which domain/subdomain should be the focus of development? This depends on which parts of the care journey the staff member/target audience is involved in as part of their role.
- Topics: What could the development focus on to ensure an impact on service delivery and AMR?
Some staff might already be familiar with AMR and AMS and will look at more specific knowledge and skills, while others need to start with the foundations of AMR and AMS to gain basic knowledge and skills.
You can find further information on how the framework can be used on the Antimicrobial Resistance and Stewardship Zone on Turas Learn.
Implementation
The framework is hosted on the Antimicrobial Resistance and Stewardship Zone on the Turas Learn platform. It can be freely accessed; no account or login is required.
Workforce departments and line manager networks should widely publicise the framework within organisations. Staff should be encouraged to actively use the framework in staff reviews and conversations.
The framework can also be used to inform further and higher education curricula, to embed antimicrobial stewardship in the training of the future healthcare and social care workforce in Scotland.
Progress on the implementation of the framework will be reported to Scottish Government. This will support the UK 5-year action plan for antimicrobial resistance 2024 to 2029.
Key implementation steps
To achieve the aims of the framework, it is crucial that its implementation is widely supported both nationally and locally.
Everyone using the framework can:
- Raise awareness of the framework through local and national networks and/or staff/line manager/supervisor communications.
- Develop local organisational strategies for embedding the framework, e.g. via local leads or champions.
- Highlight how national and local learning resources support AMS and encourage AMS learning.
Provide feedback on the framework, how it has been used and how it can be improved via the feedback form on Turas Learn or by sending an email to hai@nes.scot.nhs.uk.
Other related frameworks
This framework links to many other frameworks, and some relevant examples are listed below. It is not intended to replace any general or specialist educational frameworks already in existence, but to supplement and enhance them.
The Framework for Continuous Learning in Social Services
The Continuous Learning Framework sets out what workers in the social services need to be able to do in their job now and in the future. It describes what employers need to do to support them.
The framework for Social Work education in Scotland
There are learning requirements that each programme of social work education in Scotland must meet. They are set out in The framework for Social Work education in Scotland. These learning requirements form the Standards in Social Work Education (SiSWE).
Healthcare Support Worker Development and Education Framework for Levels 2 – 4 Healthcare Science Healthcare Support Workers
The NES Healthcare Science development and education framework supports the development of core knowledge, skills and behaviours at the support worker level. It covers the healthcare science pillars of practice.
Leading Excellence in Care Education and Development Framework
The aim of the LEiC Education and Development Framework is to support the implementation of Excellence in Care into practice. It provides guidance for the education and development of nursing, midwifery and allied health professions (NMAHP) leaders.
Nursing, midwifery and allied health professionals (NMAHP) development framework
The NES NMAHP development framework is an interactive online resource comprising of two linked parts: The Healthcare Support Workers Learning Framework and The NMAHP Post-registration Development Framework.
GP Curriculum – Royal College of Physicians
The GP Curriculum sets out the educational framework that forms the basis of GP specialty training. The curriculum sets the foundation for career-long development. It provides a full description of the knowledge, skills, attitudes and behaviours required of a GP in managing patients and their problems.
Public Health Skills and Knowledge Framework (PHSKF)
The Public Health Skills and Knowledge Framework (Public Health England 2016) is a generic framework for functions and activities for the public health workforce. It applies across the UK.
Advanced Pharmacy Framework (APF)
The RPS Advanced Pharmacy Framework (APF) is a framework for identifying and recognising the stage of practice. It supports professional development across the pharmacy profession and applies to all sectors and UK nations.
Royal Pharmaceutical Society: A Competency Framework for all Prescribers
The Competency Framework for all Prescribers has been developed for multi-professional use. It brings prescribing professions together to ensure consistency in the competencies required of all healthcare professionals carrying out the same role.
Values and behaviours
Underpinning principles
Many aspects of practice covered in other professional frameworks have intentionally not been included here, unless competencies add value in a specific context related to AMR or AMS.
The following list highlights some of the underlying key principles that are implicit in and apply to all parts of the framework:
- Person-centred care
- Collaboration and joint/partnership working
- Compassionate leadership
- Value-based prescribing
- Sustainability action
- Realistic medicine.
| Previous page 03 - Background |
Next page 05 - The framework |
