Supporting Staff
Defined as staff in supporting health or social care roles who interact with those in care or their carers, but who are not involved in direct care. Examples are receptionist, medical secretaries, porters transporting those in care, etc. These are staff who might speak to those in care, or their families or carers, answer questions, receive requests or complaints, etc.
Please refer to the framework document for a full list of statements for all domains and staff groups.
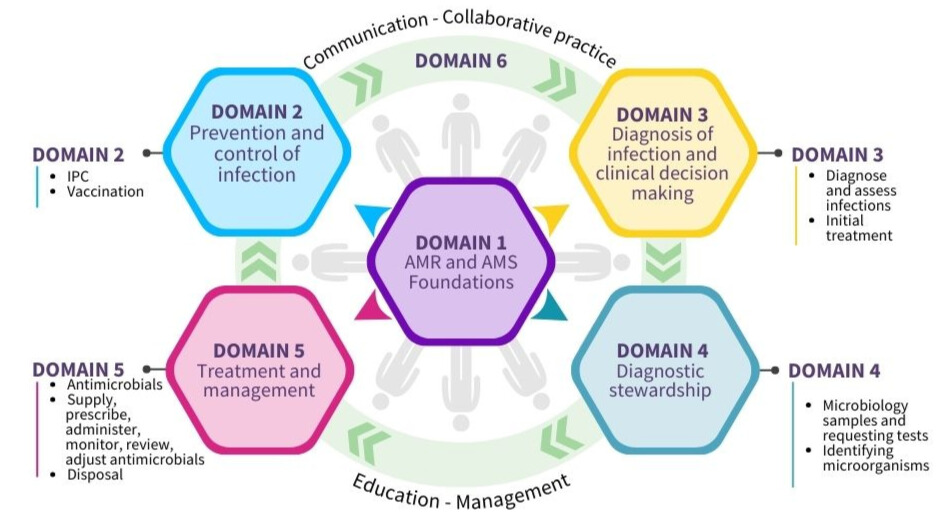
Domain 1: Foundations - awareness of antimicrobial resistance and antimicrobial stewardship
Domain 2: Prevention and control of infection
Domain 3: Diagnosis of infection and clinical decision-making
Domain 4: Diagnostic stewardship
Domain 5: Treatment and management - appropriate use of antimicrobials
Domain 6: Communication, education, collaborative practice and management
Domain 1: Foundations - awareness of antimicrobial resistance and antimicrobial stewardship
Competency
Staff can demonstrate the following knowledge and awareness of Antimicrobial Resistance (AMR) and Antimicrobial Stewardship (AMS) and how this applies to their role and care setting.
| Antimicrobial Resistance |
|---|
|
1.1 Explain what antibiotics and other antimicrobials are and why they are important. |
|
1.2 Explain what AMR is and what causes it to develop. |
|
1.3 Describe how using antimicrobials incorrectly can cause AMR. |
|
1.4 Recognise that it is important not to use antimicrobials if they are not needed, especially those that affect a wide range of bacteria (broad spectrum). |
|
1.5 Recognise that the spread of microorganisms in the community and in hospitals can greatly increase infection rates, leading to the use of more antibiotics and higher AMR. |
| Impact of AMR |
|
1.6 Explain why AMR is a serious global health threat, because it can lead to more illness, deaths, and economic problems. |
|
1.7 Identify the positive and negative effects of using antimicrobials in humans. |
|
1.8 Recognise that AMR can harm individuals and also affect entire communities or populations. |
|
1.9 Describe how using antimicrobials incorrectly can harm the environment, including the damage caused by improperly disposing of drugs and the environmental benefits of switching from intravenous (IV) to oral antimicrobials. |
| Promoting prevention of AMR |
|
1.10 Encourage health and care workers, those in care, and the public to be aware of AMR and the proper use of antimicrobials. |
|
1.11 Highlight the importance of prevention and control of Healthcare Associated Infections (HAIs) and AMR. |
| Links between IPC, AMR and AMS and patient safety |
|
1.12 Explain how infection prevention and control (IPC), AMR, AMS, and the safety of people in care are connected. |
|
1.13 Raise awareness of the connection between AMS and IPC. |
| Antimicrobial stewardship |
|
1.14 Explain what AMS means and why it is important to protect antimicrobials. |
|
1.15 Recognise that using antimicrobials responsibly is essential to stop AMR from developing and spreading. |
|
1.16 Recognise that people with viral infections and bacterial infections that go away on their own (self-limiting infections) will not benefit from taking antibiotics. |
| Roles and responsibilities |
|
1.23 Recognise their own role in AMS and consider any changes they can make in their practice to improve care and outcomes for those they care for and the public. |
|
1.24 Describe the roles, responsibilities, and skills of other health and social care workers – for example clinical nursing - involved in managing infections and AMS activities. |
|
1.25 Describe the roles and responsibilities of various members of AMS teams in managing and promoting responsible antimicrobial use. |
Domain 2: Prevention and control of infection
Competency
Staff can demonstrate an understanding of the importance of IPC and apply the principles in practice to reduce the spread of infection and AMR.
Infection prevention and control (IPC)
| SICPs and TBPs |
|---|
|
2.1 Explain what is meant by Standard Infection Control Precautions (SICPs) and Transmission Based Precautions (TBPs), and when to use them. |
|
2.2 Show how to use SICPs and TBPs in their health and/or social care working environments. |
| Role modelling and conduct |
|
2.3 Set a good example for other health and care workers and the public by following IPC principles and encouraging best practice. |
|
2.4 Explain how actions like getting the right vaccinations or staying home when sick help reduce the spread of infection and protect people they care for and other health and care workers. |
|
2.5 Recognise that health and social care staff have a duty to follow and encourage best practice for IPC. |
| Barriers and enablers |
|
2.6 Identify what makes good infection control easier or harder and know how to speak up if there is a problem. |
| Screening |
|
2.7 Explain why it is important to check for infections, (e.g. Methicillin-resistant Staphylococcus aureus (MRSA), when someone is admitted to hospital to help prevent the spread of infections. |
| Healthcare Built Environment |
|
2.8 Describe how the healthcare built environment affects IPC and the development of AMR. |
| IPC strategies |
|
2.9 Use methods and strategies to prevent and control HAIs, including infections from surgery, catheters, pneumonia, stomach flu, and others. |
|
2.10 Describe why it is important to have strategies to prevent infection in both community and healthcare settings, such as clean water, proper sanitation, waste management, and vaccinations. |
| IPC culture |
|
2.11 Develop and support the IPC culture in the workplace. |
| Challenging poor practice |
|
2.12 Recognise when infection control practices are not being followed properly and address it in the right way. |
| Healthcare and community associated infections |
|
2.13 Explain the difference between HAIs and community associated infections and their impact. |
Vaccination
| Role of vaccination |
|---|
| 2.17 Describe how vaccines help prevent infections and lower the risk of antimicrobial resistance (AMR). |
| Communication |
|
2.18 Identify strategies to boost vaccine confidence, such as providing clear, accurate information, addressing concerns and misconceptions, involving trusted healthcare professionals, and sharing positive testimonials from others who have been vaccinated. |
Domain 3: Diagnosis of infection and clinical decision-making
Competency
Staff can demonstrate an understanding of how infections are diagnosed and use this knowledge to support effective initial treatment as appropriate for their role.
Diagnosing and assessing infections
| Resistant microorganisms |
|---|
| 3.1 Explain what an antimicrobial resistant organism is. |
Domain 4: Diagnostic stewardship
Competency
Staff can initiate, carry out and demonstrate an understanding of the role of appropriate microbiology sampling and testing to inform diagnosis and treatment of infections as appropriate for their role.
Microbiology samples and requesting tests
| Diagnostic stewardship |
|---|
|
4.1 Explain the principles and practice of diagnostic stewardship: Right test - right person - right time. |
|
4.2 Support the implementation of diagnostic stewardship in their own role. |
| Microbiology samples - general |
|
4.3 Describe their role in the identification, collection, handling, transportation and reporting of microbiological samples and test results. |
| Taking microbiology samples |
|
4.7 Follow the correct procedures for choosing, collecting, storing, and transporting samples to the lab, according to the right policies and guidelines, and complete all necessary information, like clinical, demographic, and other relevant details, for each sample. |
Identifying microorganisms
| The role of the laboratory |
|---|
|
4.9 Describe how the microbiology laboratory helps to identify microorganisms and resistance patterns, supports case management, and provides information for IPC and AMS. |
| Reporting test results |
|
4.10 Make sure samples are handled quickly and within the required time frame. |
Domain 5: Treatment and management - appropriate use of antimicrobials
Competency
Staff can safely supply, prescribe, administer, monitor, review, adjust, and dispose of antimicrobials according to best practice guidelines as appropriate for their role.
Supply and disposal
| Disposing antimicrobials |
|---|
|
5.76 Dispose of unused antimicrobial medicines safely. |
Domain 6: Communication, education, collaborative practice and management
Competency
Staff can effectively collaborate and communicate with co-workers, the wider team and those they care for and their families/carers, provide educational support on the use of antimicrobials and promote stewardship activities as appropriate for their role.
Communication and education
| Communication |
|---|
|
6.1 Recognise the importance of communicating with people they care for and other staff. |
| Communication with clinicians |
|
6.5 Maintain effective communication and work together with doctors, antimicrobial management teams, IPC professionals, hospital epidemiologists, and other health and care workers involved in AMS activities. |
|
6.6 Explain why it is important to work with experts, like infection specialists, when their help is needed. |
| Education on safe and appropriate use of antimicrobials |
|
6.17 Encourage ways to help individuals or communities learn how to use antimicrobials correctly. |
| Education - when antimicrobials are not needed |
|
6.20 Educate those they care for and their carers, and other supporting clinical staff about: • self-care (based on evidence, for example with pain relief, rest, and fluids) |
| Education - identify learning needs |
| 6.22 Identify their own learning needs and goals for development in AMS. |
Collaborative practice and management
| Team working |
|---|
|
6.23 Get involved in AMS as part of a team with members from different areas of expertise. |
|
6.24 Explain why it is important for healthcare professionals involved in giving antimicrobials (like prescribing, delivering, and supplying) to all understand the same antimicrobial treatment policy decisions, the quantity/quality of antimicrobial use, and what results are expected. |
|
6.25 Ask for help and advice from the AMS team when necessary. |
|
6.26 Work with the AMS team to help ensure antibiotics are used in the best way. |
| Prioritisation of AMS |
|
6.30 Support public health campaigns about AMR, for example:
|
| Previous page 04 - About the framework |
Next page 06 - Education to support the framework |
